Do you find yourself going to the restroom frequently throughout the day or waking up multiple times a night to urinate? Do you experience sudden urges to urinate, sometimes accompanied by episodes of urine leakage?
If your answer to either of these questions is yes, you may be suffering from overactive bladder (OAB). But don’t worry – you are not alone. Though OAB is an abnormality and should not be ignored, it is a common condition, affecting about 50 million people in the United States. That includes 40 percent of women and 30 percent of men.
Because overactive bladder is most common in those over the age of 65 (or 40 for women), many people think overactive bladder is just a normal part of aging. However, this is not the case. In fact, OAB can even alert you to more serious problems – and it is a treatable condition.
The first step to getting treated is recognizing the signs of overactive bladder. Keep reading to learn more about what overactive bladder is, what causes it, and the symptoms that accompany it.
What is overactive bladder?
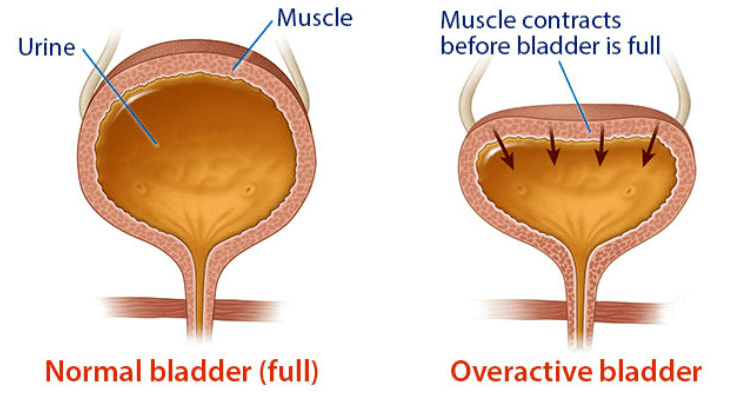
In general, OAB is a problem that affects the bladder’s ability to hold urine. As a healthy bladder is filled with urine, it stretches and expands to accommodate the increased volume. Specialized nerves in the bladder lining can then sense when the bladder is full and signal to the brain that it is time to empty.
In the normal situation, you are able to voluntarily control when to empty the bladder – that is, you note the sensation of needing to urinate and are able to hold it until you get to the bathroom. You voluntarily relax your pelvic floor muscles, allowing the urine to exit the bladder.
For people with OAB, however, there is thought to be abnormal communication between the brain and the bladder such that the bladder muscle contracts involuntarily. Thus, they may experience a strong, sudden urge to urinate even when the bladder volume is low. This can lead to not only frequent urination, but also involuntary urine leakage (incontinence).
OAB can be further categorized into two types: dry and wet. In OAB dry, incontinence is not present, whereas in OAB wet, sudden urges to urinate can be accompanied by leakage. To get an accurate diagnosis, it’s important for patients to communicate their symptoms clearly to their doctors no matter how uncomfortable it may be.
How do I know if I have OAB?
It’s important to note that the symptoms and signs of overactive bladder can differ from person to person and fluctuate over time, so it is not always easy to spot the condition right away. However, the most common signs of overactive bladder include:
- Frequent urination throughout the day (more than 8 times in 24 hours)
- Waking up multiple times per night to urinate
- Sudden urges to urinate, sometimes accompanied by involuntary leakage (urinary incontinence)
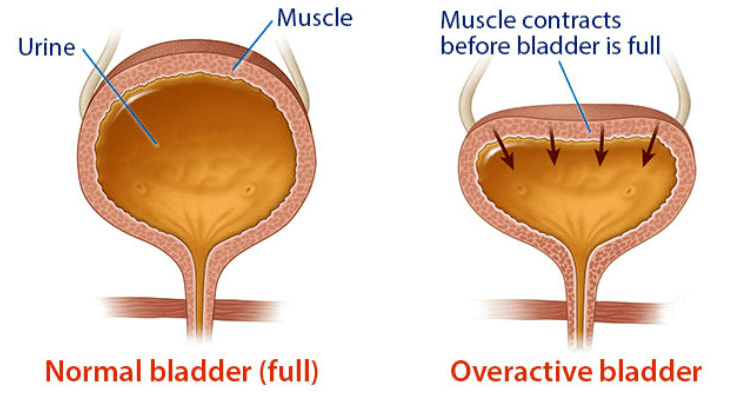
The above illustration shows the difference between a normal bladder that’s full and an overactive bladder.
What is the main cause of overactive bladder?
Part of what makes OAB tricky to spot and treat is that it has a variety of potential causes. However, many causes stem from problems with the urinary tract. If you do experience symptoms of OAB, it is important to discuss them with your doctor so that you may be alerted to any potential problems with your urinary tract health.
Other main causes of OAB include:
- Medications that increase urine production
- Drinking an excess of fluids
- Consumption of diuretics such as caffeine or alcohol
- Urinary tract infections
- Diabetes
- Other bladder conditions, e.g., bladder stones or bladder cancer
- Certain neurological conditions
OAB and quality of life
OAB can significantly disrupt your quality of life, including disruptions to your sleep and sometimes an exacerbation of conditions like depression and anxiety. Suffering from embarrassing leaks or constantly having to schedule your day around proximity to a restroom can cause undue stress and make it difficult to function in work and life.
Fortunately, you do not have to live with this condition. Several treatment options exist to help manage your OAB symptoms. The first step is communicating with your doctor and obtaining the right diagnosis.
Diagnosing symptoms of overactive bladder
Someone experiencing the signs of overactive bladder should contact their primary care doctor. Doctors typically perform several tests to rule out other conditions, including urinalysis, physical exam, bladder scan, urodynamic testing, or cystoscopy. Doctors may also refer patients to urologists, who specialize in bladder tissue health.
How is OAB treated?
There are essentially three levels of treatment along the OAB patient care pathway. As with many health conditions, the treatment pathway for those with OAB begins with conservative options and moves on to the most intensive interventions:
- Behavioral Interventions
- Medication
- Advanced Therapies
Behavioral Interventions for OAB
Behavioral interventions are recommended as the first level of treatment, as they are the least invasive and resource intensive. These can include:
- Exercises to strengthen your pelvic floor muscles, e.g., Kegel exercises
- Maintaining a healthy body weight
- Modification to your diet, e.g., avoiding spicy foods
- Modifying yourfluid intake, including drinking fluids in moderation or avoiding caffeine and alcohol
- Bladder training
- Keeping a bladder diary to track symptoms
Medication for OAB
If behavioral changes are unable to provide symptom relief, you may need to move to the next level of treatment: medications. The goal of these medications is to help relax your bladder so you have more control of your pelvic floor muscles and go less often.
Advanced Therapies for OAB
If symptom relief is still not achieved or you experience unwanted side effects from the medications, third-line advanced therapies may be the solution. These include surgeries, devices, and other specialized therapies, including Sacral Neuromodulation, Botox®*, and Percutaneous Tibial Nerve Stimulation (PTNS).
Axonics® Solutions
Axonics Therapy is a clinically proven long-term therapy that helps restore normal communication between the brain and the bladder, which may reduce or eliminate OAB symptoms.
If you think you are showing signs of overactive bladder, talk to your doctor about your symptoms. Together, you can find the right treatment solution to regain control.
Need help finding a doctor? The Axonics® Find Real Relief Advisor Team is here to assist you. It only takes minutes for us to connect you with a physician near you who might change your life. Complete the survey below to find a bladder specialist near you.
To learn more about living with an overactive bladder, including tips and info, check out the Axonics® Therapy Blog.
Take The Quiz. Find A Specialist.
Axonics® Privacy Policy
Axonics, Inc. has created this Privacy Policy to document and demonstrate our firm commitment to privacy. This Privacy Policy describes the ways in which Axonics and its affiliates, service providers, and subsidiaries (collectively, “Axonics,” “we,” “our,” or “us”) may collect, use, and disclose personal information obtained or gathered through the use of Axonics websites or services that link to this policy (the “Services”). By using the Services and/or disclosing personal information, you consent to the processing of your personal information as set forth in this Privacy Policy, which is incorporated into our Terms of Use. This Privacy Statement is intended for website users in the United States. We will not sell the personal information that you provide to us.
What Information Do We Collect?
There are various places on the Axonics website where you can elect or sign-up to receive information from Axonics. We may collect the following categories of personal information about you in connection with your use of the Services:
Information You Provide: We and our Service providers collect personal information that you may voluntarily share when you use the Services, including, but not limited to, information about your:
- Contact information, such as your first name, last name, email address, address, phone number;
- Demographic information, including your age, birth date, and gender;
- Professional information, including your employment status, employer information, title, occupation, and professional affiliations;
- Account information, including your username and password;
- Health information, including your health status, diagnoses, treatments, and symptoms;
Information Automatically Collected From You: We and our service providers may automatically collect certain information about you and your online activities when you use the Services. We may collect personal and non-personal information, including, but not limited to, your Internet Protocol address, general geographic location, browser type, operating system, the pages you view on the Services, the pages you view immediately before and after you access the Services, links you follow on our website, and the search terms you enter on the Services.
How Do We Use Your Information?
We may use the information we collect for a number of purposes, including:
- to provide you with products, services, or information you request;
- to provide you with information about the Services or required notices;
- to deliver marketing communications, promotional materials, or advertisements that may be of interest to you;
- to customize your experience when using the Services, such as by providing interactive or personalized elements on the Services and providing you with content based on your interests;
- to improve the Services, such as by better tailoring our content to our users’ needs and preferences;
- to generate and analyze statistics about your use of the Services;
- to answer your questions about the Services, or otherwise communicate with you about the Services;
- for our business purposes, such as monitoring and prevention of fraud, intellectual property infringement, violations of our Terms of Use, violations of law, or other potential misuse of the Services.
When and to Whom Do We Disclose Your Information?
The information that we collect from and about you may be used internally by Axonics and may also be disclosed:
- to third parties that provide services to us in connection with our business operations and that have agreed to keep the information confidential;
- to business partners who offer products or services jointly with us or with our subsidiaries or affiliates;
- as required by law, such as to comply with a subpoena or other legal process, or to comply with government reporting obligations;
- when we believe in good faith that disclosure is necessary (a) to protect our rights, the integrity of the Services, or your safety or the safety of others, or (b) to detect, prevent, or respond to fraud, intellectual property infringement, violations of our Terms of Use, violations of law, or other misuse of the Services; and
- to service providers, advisors, potential transactional partners, or other third parties in connection with the consideration, negotiation, or completion of a corporate transaction in which we are acquired by or merged with another company or we sell, liquidate, or transfer all or a portion of our assets.
Use of Cookies
To enable us to provide customized and personalized services, we and our service providers use cookies and similar tools to store and sometimes track information about you. A cookie is a small amount of data that is sent to your browser from a Web server and stored on your computer. If you do not want the Services to collect information through the use of cookies, you can set your web browser to reject cookies. Each browser is different, so you should check your browser’s “Help” menu to learn how to change your cookie preferences. If you reject or block cookies from the Services, however, the Services may not function as intended.
Use of Google Analytics
Google Analytics uses cookies to track your interactions with our website and online Services. Google then collects that information and reports it back to us. For more information on Google Analytics, visit “HOW GOOGLE USES INFORMATION FROM SITES OR APPS THAT USE OUR SERVICES” located at: https://www.google.com/policies/privacy/partners/.
Do Not Track Signals
California law requires that we share how we respond to website browser “do not track” signals. We do not currently recognize or honor “do not track” signals or other mechanisms that provide a method to opt out of the collection of information across websites or other online services. If we do so in the future, we will describe how we do so in this Privacy Policy. Visit the following website, www.allaboutdnt.org, for more information.
Your California Privacy Rights
If you reside in California and have provided your personally identifiable information to us, you may request information once per calendar year about our disclosures of certain categories of your personally identifiable information to third parties for their direct marketing purposes. Such requests must be submitted to us in writing at
This email address is being protected from spambots. You need JavaScript enabled to view it..
Children's Information
The Services are not intended for or directed to individuals under the age of thirteen (13). If a parent or guardian becomes aware that his or her child has directly provided us with personal information, please contact us by using the contact information below.
Changes to This Privacy Policy
We may update this Privacy Policy from time to time. If we update this Privacy Policy, we will notify you by posting a new Privacy Policy to this page. If we make a material change to our Privacy Policy, we will take reasonable steps to notify you, for example by posting a banner on the Services website, prior to putting the changes into effect.
Contact Us
If you have any questions, please contact us at This email address is being protected from spambots. You need JavaScript enabled to view it..
Effective Date: July 8, 2019